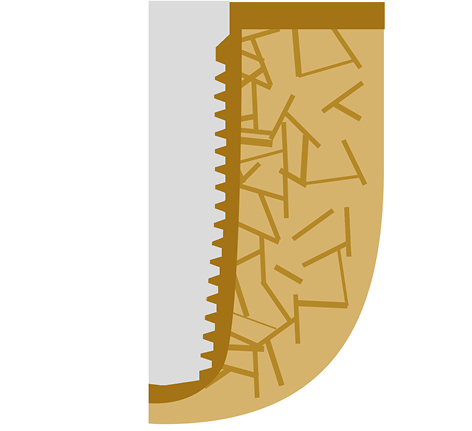
Fig 1 illustrates an implant inserted to achieve “osseointegration”. The crestal cortical bone and the spongious bone will (must) develop now more bone on the implant’s surface. A procedure that takes 3-6 or more months. To ensure that all the necessary processes will happen, enough spongious bone must be available between the endosseous surface of the implant and the outer cortical to secure the constant supply of nutrients to the repair site. The implants will be integrated partly in woven bone and later into the newly formed osteonal bone.
Internationale Implantatstiftung
Wir sind eine gemeinnützige und wissenschaftlich ausgerichtete Stiftung des Privatrechts, die Patientenerfahrungen und Ergebnisse von
Zahnimplantat-Versorgungen nach Knochenaufbau
erfassen und bewerten möchte.
Ziel ist die Erstellung einer Studie zur dentalen Versorgungsrealität in Deutschland / Österreich / Schweiz.
Einsender (Patienten u.a.) erhalten eine fachliche Einschätzung und Bewertung, kostenfrei und vertraulich.
Bitte wenden Sie sich an:
Internationale Implantatstiftung München
contact@implantfoundation.org
4th IF® Consensus Document for Oral Implantology: Description of Methods to Create Permanent Bone-to-Implant Contact. Clinical Indications and Modalities for these Methods.
(2022, Version 2)
© 2022, International Implant Foundation, Munich/Germany
Authors of this 2nd, revised version: IF Board. This Consensus Document replaces Version 1 of the same document, which has been published in 2012.
First consultation period for interested parties: October 5th 2021 until April 5th 2022
Applicable documents: All IF Consensus Documents No. 1-8; AO Principles of Fracture Management; THOMAS P RÜEDI, RICHARD BUCKLEY, CHRISTOPHER G MORAN; ISBN 9781588905567
Scope: Lateral and screwable oral and craniofacial implants according to IF Consensus Document No. 1
Historic background: During the period from 1990 until approximately 2020, the concept of “Osseointegration” dominated the dental implant market. Implants underwent osseointegration during a “healing period” of 3-6 months, depending on the primary stability achieved during surgery. The implant surface roughness or topography was assumed to influence the bone’s healing positively, but didn’t advocate immediate functional loading in regular cases. On the other hand, before this period (1956-approximately 1990), implantologists tended to use polished or machined surface implants, as they tried to bring their implants in intimate cortical contact to achieve cortical support. A treatment approach that was typically followed in immediate functional loading protocols, and single-piece implants.
This consensus document describes all the possible approaches that can be used to achieve permanent bone-to-implant contact.
I. The Osseointegration Approach

Fig 2 illustrates the bone-implant contact region after a vertical cortical bone contact has been established along the implant body. The crestal and vertical cortical bones form one functional unit. Osseointegration is considered complete, and the (2-stage) implant can be effectively used/loaded.
The method of “osseointegration” should be considered when the primary stability prerequisite for immediate loading cannot be achieved during surgery (i.e. in most cases), and hence secondary stability is required. For optimum functioning of this method, no cortical support or cortical anchorage is required, however contact to cortical will increase the stability to an extend that even treatments in immediate functional loading are possible in some cases (e.g. All-on-4-method).
If sufficient numbers of implants are placed with satisfactory cortical anchorage and if implants are splinted immediately, often immediate functional loading is possible. As an example, the “All-on-4” modus of usage is such a method.
It has to be mentioned here that the term “osseointegration“ does not imply or include that the bone is somehow bonded to the surface of the implant. Due to the rough surfaces, an uncountable amount of mechanical retentions are created during osseointegration.
Osseointegration is, in fact, a corticalisation of the bone close to the implant’s surface. In general, the method of osseointegration is connected to a number of disadvantages (healing time, high demand of bone, development of periimplantitis and others), and today the indications for the use of this method are strongly reduced.
II. The “Compression of Spongious Bone” Approach
All endosseous implants with a conical shape design must be considered as “compression screws” implants. The drill hole into which the implant is inserted is under-dimensioned, at least in width, compared to the implants inserted later.
Fig 3 An under-dimensioned conical drill removes a minimal amount of bone, just enough to allow placement of the implant with compression force up to approximately 80 Ncm.
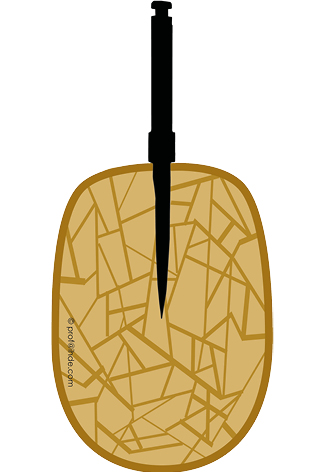
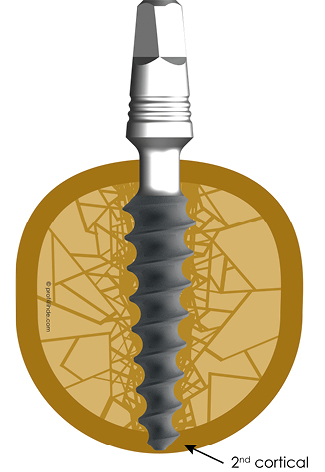
Fig 4 Subsequent to implant insertion, the spongious bone is displaced laterally and compressed both laterally and at the apex of the implant, forming a higher mineralization zone. This process has been named “corticalisation of spongious bone”. The compressed bone is not “repaired” later; it remains permanently. As soon as the implant is loaded, more cortical bone is formed as a response to the functional load. This approach provides enough stability for an immediate functional loading protocol in the jawbones with sufficient mineralization (bone quality D2, D3).

Fig 5 Whenever it is possible, the surgeon will combine the corticalisation of spongious bone with cortical support (as shown here in the caudal 2nd cortical). This figure shows the situation after a conical compression screw implant has been inserted and is receiving a caudal cortical support (against intrusive forces) by engaging the 2nd cortex.
III. Direct Cortical Engagement Approach
If implants are placed in direct contact to cortical jaw bone (under pressure), immediate loading protocols are possible. This method does not require a minimal amount of bone on the vestibular and lingual/palatal side of the implant. It is important that the cortical bone is intact and not fractured (i.e. not showing a greenstick fracture).
Fig 6 For this approach, the implant was chosen with optimum thickness and design to get direct contact with the cortical bone, with no spongious bone being present. No biologic integration of this implant will be encountered, because de-novo bone formation does not happen inside a cortical.
The placement of an implant following IF Method No. 6 is a typical example for this approach. For the success of this implant, the pre-existing cortical should be remains stable.

Fig 7 Corticobasal® Implants are anchored in the 2nd cortical bone. To achieve this bi-cortical stabilization, the surgeon will typically (fully) penetrate the second cortex. The load is transmitted into the 2nd cortical region. On the other hand, the load transmission in the 1st cortical (atrophy-prone region) is not the primary aim of the placement approach.

Corticobasal® implants follow the direct cortical engagement approach (Osseofixation). The implants are characterized by having only apical threads which anchor into the cortical bone (in bone areas where this is possible) with high primary stability. The implant provides a thin guiding tip (0.7 mml) which guides the implant during implant insertion and allows safe engagement in the 2nd/3rd cortical. This tip may be removed in order to achieve a larger amount of cortical anchorage without an overly strong penetrating apical tip. Corticobasal® implants feature isoelastic properties, and these properties depend on the nominal diameter, the length and the design of the implant. Due to these design features Corticobasal® implants differ in indication and usage significantly from traditional (2-stage) implants, which were designed for the older „Method of Osseointegration“.
IV. The Approach of “Lateral Basal Implants” and “Blade Implants”
Both the “lateral basal implants” and “blade implants” are hammered into thin slots in the bone. Implants in this approach gain their primary stability by getting their plates stuck between the corticals. After this, the bone slot is filled with woven bone. Both implant designs (lateral basal implants and blade implants) tend to fail, if the implants are not in contact with cortical bone in the final position.
V. The Immediate Functional Loading Concept Has Become the Specialist Standard in Oral Implantology
Since 1956, the immediate loading protocols have been used in oral implantology, especially in the field of maxillofacial implants. This protocol had and has a documented high success rate and may be used in almost every case and without augmentations. In contrast, delayed loading protocols have been introduced into the profession with the development of the “2-stage implants”.
The product life cycle of implants which were used according to the old Branemark protocol has ended.
Since the internet provides freely accessible information today, the majority of the patients nowadays request an immediate loading treatment protocol; hence the use of delayed loading protocols and 2-stage implants is not adequate anymore. With the spreading of the technology, sufficient treatment providers, devices and equipment are available in most countries to meet patients’ demands.
Indications
- Circular bridges
- Segment bridges
- Single tooth replacement using one CBI®
- Single tooth replacement using two CBI®
- Single tooth replacement using three CBI®
The surgical treatment provider has a vital role in determining the success of the prosthetic protocol, as only he/she knows the situation of the bone during the surgery. Moreover, the surgical treatment provider decides about the necessary amount of implants in one BIPS.
General recommendations about the number of implants per jaw (as proclaimed by several societies for implantology) are not relevant for the treatment protocol for Corticobasal® implants. Such recommendations are often influenced by health insurances and they are inacceptable from medical point of view. Health insurances are financially motivated to keep the number of implants low. Their intention is often not a full recovery of the masticatory system of their customers.
Additionally, the surgical treatment provider should consider increasing the number of the points used for cortical engagement of the BIPS and follow the 16 proven methods and sub-methods of implant insertion and engagement.
On the other hand, the chewing forces can be reduced temporarily, e.g. through Botulinum-Toxin in the Masseter muscle, to ensure treatment success for patients with overly strong muscles and unequal chewing forces on both sides.
Using an adequate prosthetic concept with an equal number of teeth on both sides.
Planning and setting up a BIPS is a protected intellectual work.
VI. Comments on the “Difficulty” and Risks of Procedures which Include Corticobasal® Implants
An analysis of the literature shows that by the use of Corticobasal® implants (CBI®), treatment risks are strongly reduced compared to the older method of “osseointegration.”
The reasons are
- the limited number of necessary surgical interventions,
- avoiding the use of bone augmentation materials,
- use of polished implants only (no risk of periimplantitis).
In the field of Corticobasal® implants, 16 approved methods and sub-methods are applied. Therefore, the surgeon has a clear guideline for implant placement, and all cases treated with standard segments and circular bridges can be considered “not difficult”. This is especially true because the training of implantologists for their work in the field of Corticobasal® implants is structured in a curriculum. After undergoing curriculum training and other follow-up trainings, the (former) dentist is considered a trained treatment provider for Corticobasal® implants. No other training or a specialty as an oral surgeon are necessary.
VII. Comments on the Necessary Qualification for Treatment Providers
The demand raised by some associations that “only oral surgeons can place implants” is unacceptable and not backed by any evidence because the risks of the procedures used when applying Corticobasal® implants are known to be extremely low. In some countries (e.g. Russia and Ukraine), only specialized “stomatology chirurgs” may extract teeth and do oral surgery. For oral/dental implants placement, such specialization is required, e.g., in Russia and Ukraine. The amount of training for this “specialization” is considerably low and it includes mainly a concentrated repetition of teaching during studies at the universities. In Russia and Ukraine such specialisations have to be retaken every five years. This shows that also for the technology of Corticobasal® implants a planned repetition of teaching (as demanded by the manufacturers) is adequate. The amount of knowledge transferred to a “stomatology chirurg” resembles the amount of knowledge transferred in a typical curriculum training for Corticobasal® implants.
To become an oral surgeon, in most countries a 3-year in-house training is necessary. This amount of knowledge and qualification is unnecessary for treatment providers who plan to carry out treatments with Corticobasal® implants. In western countries, specializations like “stomatology chirurg” are not available.
Index for Changes in Rev. 2 of the IF Consensus Document No. 4
| Revision No. | Document name / number | New version | Previous version | Modification | Date of approval | Release by |
|---|---|---|---|---|---|---|
| 0 | EN_Consensus_for_implantology_to_achieve_osseointegration_04-22_V002 | V002 | - | - | 07.04.2022 | IF Board, for consultation |




